Plasmodium
Classification of Animals Non Chordates of Class 11
Plasmodium
Discovered in RBCs of man by Charles Laveran while Sir Ronald Ross observed oocysts of Plasmodium on the stomach wall of female Anopheles mosquito.
Out of about 60 species, only four species cause malaria in man.
Plasmodium is a digenetic, intracellular parasite found in the blood of man.
Asexual cycle occurs in man by a process called Schizogony (in liver and RBCs). Schizogony is a type of multiple fission.
Sexual cycle is completed in mosquito by gametogony and sporogony.
Infective stage of Plasmodium - sporozoite.
Geographical Distribution
Found in all countries but tropical zone is the endemic home of all malarial parasites.
P. malariae is a parasite of subtropical zone while P. vivax is the prevailing species of the temperate zone.
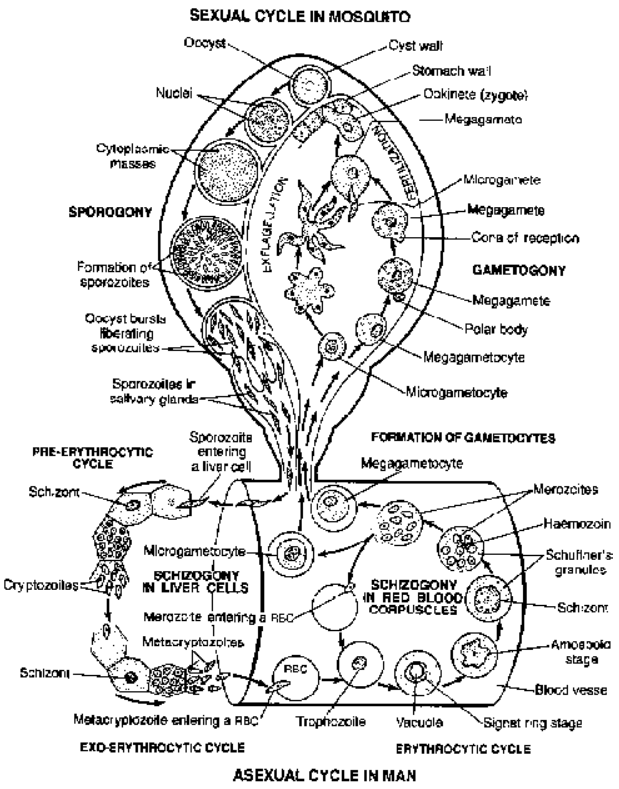
Fig. Life cycle of Plasmodium vivax
Habitat : Malarial parasites infecting man, after passing through a developmental phase in the parenchymal cells of liver, reside inside RBCs and are carried by the circulating blood to all the organs.
Human Cycle
Occurs inside parenchyma of liver during which Plasmodium schizont undergo a phase of development.
Liberated merozoites are called cryptozoites. Smaller ones (micromerozoites) enter the circulation and the larger ones (macromerozoites) re-enter the liver cells to undergo schizogony.
During this phase, it cannot be detected in blood samples and do not produce any clinical symptoms.
(ii) Erythrocytic Schizogony
It resides inside RBC and passes through stages of trophozoite, schizont and merozoite.
After entering into an erthrocyte, a merozoite becomes a rounded disc-like young trophozoite. As it grows, large vacuole appears in the centre to push the nucleus towards the periphery. This forms signete ring
shape.
The trophozoite becomes amoeboid by loosing its vacuole. Now it starts feeding more actively upon cytoplasm of host RBC. It secretes out lysolecithin enzyme to dissolve the cytoplasm of RBC. The
trophozoite becomes brownish black haemozoin granule formed due to proteolysis of haemoglobin.
Haemoglobin breaks down into globin (protein) and the red pigment hematin (which accumulates in trophozoite’s cytoplasm).
In the cytoplasm of RBC Schuffner’s dots are observed.
The mature trophozoite undergoes repeated mitotic divisions to form 8 to 26 daughter nuclei. The daughter nuclei migrate close to its periphery and it separated out with small amount of cytoplasm. These small
cells are called merozoites.
When RBC bursts it releases merozoites and haemozoin crystals. The liberated merozoites attack fresh RBCs whereas haemozoin crystals causes malarial fever.
These asexual forms can be detected in peripheral blood 3 to 4 days after the completion of pre-erythrocytic schizogony.
Parasitic multiplication in RBC during this phase produces clinical attack of malaria.
(iii) Gametogony
Some merozoites after completing erythrocytic schizogony, instead of developing into trophozoites and schizonts, give rise to forms which are capable of sexual reproduction after leaving the human host. These
are called gametocytes and develop in the RBCs of the capillaries of internal organs (spleen and bone marrow).
Only mature gametocytes are found in the peripheral blood.
The gametocytes which have entered mosquito are two types, microgametocyte and megagametocyte.
The individual who harbours the gametocytes is known as ‘carrier’.
(iv) Exo-erythrocytic schizogony
After establishment of blood infection, the pre-erythrocytic phase disappears completely.
Exo-erythrocytic forms are responsible for relapses of vivax, ovale and quartan malaria.
Mosquito cycle/sexual cycle of malarial parasite
Sexual cycle first starts in the human host by the formation of gametocytes which are then transferred to the insect host where further development proceeds.
Female Anopheles during its blood meal from an infected person, ingests both sexual and asexual forms but only sexual forms are capable of development and the rest die off immediately.
First phase of development occurs inside the midgut (“stomach”) of the mosquito. From one microgametocyte, 5-8 thread - like filamentous structures, microgametes develop. This is called ex-flagellation.
Macrogametocyte do not show any flagellation and from one macrogametocyte only one macrogamete is formed.
Gametes undergo fertilization and form ookinete; which upon entry into the mucosal cells form oocyst.
Oocyst increases in size and undergo meiotic and mitotic divisions to form large number of haploid sporozoites. Sporozoites are distributed through the circulating fluid (Haemocoel) into various organs and
tissues of the body. Maximum number accumulates in salivary duct.
Mosquito at this stage is capable of transmitting infection to man.
Spread of Malaria : factors responsible include:
(i) Presence of a gametocyte carrier (source of malarial parasite).
(ii) Existence of a suitable Anopheles vector.
(iii) A susceptible person.
Incubation period : Sporozoites on gaining entrance into the human body undergoes a developmental cycle first in liver and then in RBC. With the commencement of erythrocytic schizogony the parasite
multiplies in geometric progression and on reaching a sufficient concentration in the blood, brings about the onset of fever. This period of development is called incubation period.
In P. vivax, P. ovale and P. falciparium : 10-14 days and in P. malariae it is 18 days to 6 weeks.
Clinical Symptoms of Malaria
The main clinical manifestations are series of intermittent fever, followed by anaemia and splenic enlargement.
(i) Malarial fever : May occur at any time but generally starts in early afternoon. It is divided into 3 stages
▶ The cold stage (lasting 20 minutes to an hour)
▶ The hot stage (lasting 1 to 4 hours)
▶ The sweating stage (lasting 2 to 3 hours)
Malarial fever synchronises with the erythrocytic schizogony of the malarial parasite and relapses may vary with the type of species:
(a) With 48 hour cycle fever recurs every third day : tertian fever
(b) With 72 hour cycle fever recurs every fourth day : quartan fever.
Treatment :
Various antimalarial drugs are grouped as
1. Therapeutic (Clinial cure) : 4-aminoquinolines like chloroquine and amodiaquine, and mepacrine are potent schizonticidal drugs having action on early erythrocytic phases of the parasite.
2. Protective or Prophylactic
Proguanil, pyrimethamine and trimethoprim are used to suppress clinical manifestations. These drugs destroy pre-erythrocytic phase of the parasite in the liver and inactivates gametocytes, thereby preventing
further development in the mosquitoes.
3. Synergists : They potentiate the action of schizonticidal drugs. Sulphonamides and sulphones (dapsone) are often used in combination with prophylactic drugs.